About CSCS
Disclaimer: this app is designed by and for ovarian cancer surgeons. If you downloaded this application as a patient please talk to your doctor for advice.
The aim of this APP is to help doctors in the prognosis of the achievement of suboptimal surgery in the surgical treatment of advanced ovarian cancer, with the possible repercussion that this could have on the choice of the most appropriate therapeutic strategy.
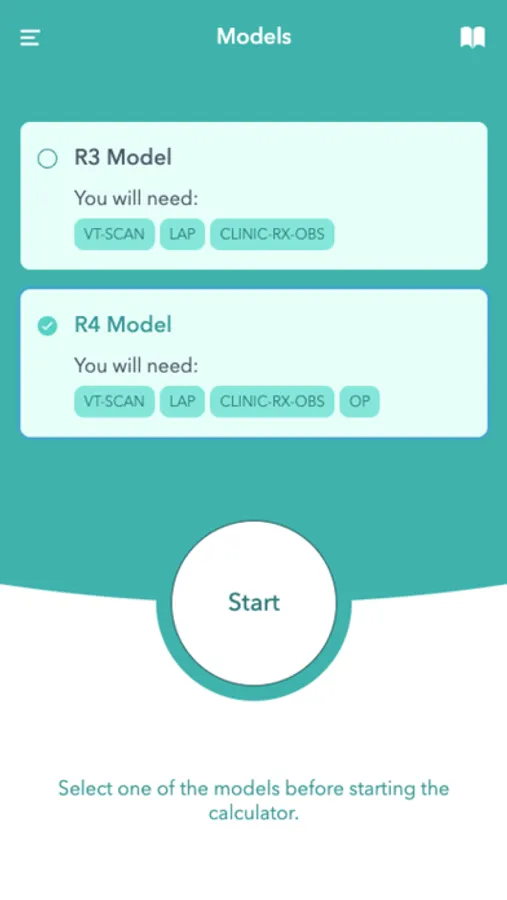
We present 2 prognostic models, R3 and R4, based on the determination of the Peritoneal Carcinomatosis Index (PCI) obtained in the preoperative period with the Computerized Axial Tomography (CT-scan), the PCI obtained by Laparoscopy staging, the one obtained in the surgical exploration of the peritoneal cavity (operative PCI), as well as in the existence of intestinal obstructive signs in any of the aforementioned diagnostic tests. The R3 model includes exclusively pre-operative diagnostic tests: CT-scan and Laparoscopy if it had been performed, and the possible signs of total or partial intestinal obstruction. The R4 model adds to the above the result of the operative PCI.
The models R3 and R4 can be considered as a diagnostic test that encompasses the other mentioned tests. As such, they have their own Sensitivity and Specificity, and establish an initial prognosis based on these diagnostic indices. But obtaining a definitive diagnosis (Final Prognosis or Positive Predictive Value) of the possibility of suboptimal surgery requires the integration of the prevalence of existing suboptimal surgery, according to the general formula of Bayes' Theorem. This prevalence is represented by the percentage of suboptimal surgery that has until that moment who applies the model to their specific patient.
Every prognostic model offers explicit results along with a spectrum of uncertain results. The R3 and R4 models are no exception. Therefore, it is advised that for suboptimal surgery, a Positive predictive value of up to 35% be considered as “UNLIKELY suboptimal citoreductive surgery”, between 35% and 69% as “UNCERTAIN”, and 70% thereafter as “PROBABLE suboptimal citoreductive surgery”.
All prognostic model must be validated by each doctor that employs it, before considering it effective for its habitual use. Therefore, it is important that each user verifies the extent to which the final prognosis obtained by the model coincides with the final result of suboptimal surgery in a series of cases in which it has been applied.
The aim of this APP is to help doctors in the prognosis of the achievement of suboptimal surgery in the surgical treatment of advanced ovarian cancer, with the possible repercussion that this could have on the choice of the most appropriate therapeutic strategy.
We present 2 prognostic models, R3 and R4, based on the determination of the Peritoneal Carcinomatosis Index (PCI) obtained in the preoperative period with the Computerized Axial Tomography (CT-scan), the PCI obtained by Laparoscopy staging, the one obtained in the surgical exploration of the peritoneal cavity (operative PCI), as well as in the existence of intestinal obstructive signs in any of the aforementioned diagnostic tests. The R3 model includes exclusively pre-operative diagnostic tests: CT-scan and Laparoscopy if it had been performed, and the possible signs of total or partial intestinal obstruction. The R4 model adds to the above the result of the operative PCI.
The models R3 and R4 can be considered as a diagnostic test that encompasses the other mentioned tests. As such, they have their own Sensitivity and Specificity, and establish an initial prognosis based on these diagnostic indices. But obtaining a definitive diagnosis (Final Prognosis or Positive Predictive Value) of the possibility of suboptimal surgery requires the integration of the prevalence of existing suboptimal surgery, according to the general formula of Bayes' Theorem. This prevalence is represented by the percentage of suboptimal surgery that has until that moment who applies the model to their specific patient.
Every prognostic model offers explicit results along with a spectrum of uncertain results. The R3 and R4 models are no exception. Therefore, it is advised that for suboptimal surgery, a Positive predictive value of up to 35% be considered as “UNLIKELY suboptimal citoreductive surgery”, between 35% and 69% as “UNCERTAIN”, and 70% thereafter as “PROBABLE suboptimal citoreductive surgery”.
All prognostic model must be validated by each doctor that employs it, before considering it effective for its habitual use. Therefore, it is important that each user verifies the extent to which the final prognosis obtained by the model coincides with the final result of suboptimal surgery in a series of cases in which it has been applied.