AppRecs review analysis
AppRecs rating 3.4. Trustworthiness 76 out of 100. Review manipulation risk 20 out of 100. Based on a review sample analyzed.
★★★☆☆
3.4
AppRecs Rating
Ratings breakdown
5 star
40%
4 star
20%
3 star
0%
2 star
20%
1 star
20%
What to know
✓
Low review manipulation risk
20% review manipulation risk
✓
Credible reviews
76% trustworthiness score from analyzed reviews
About eScription One
eScription One allows authorized clinicians to create and manage high quality documentation for an EMR with minimal time and effort. Clinicians dictate the narrative and keep pace with busy patient loads without compromising time with patients, revenue potential or length of workday. Meanwhile, timely, complete, structured data in the EMR reduces claim rejections, decreases time to bill and enhances compliance.
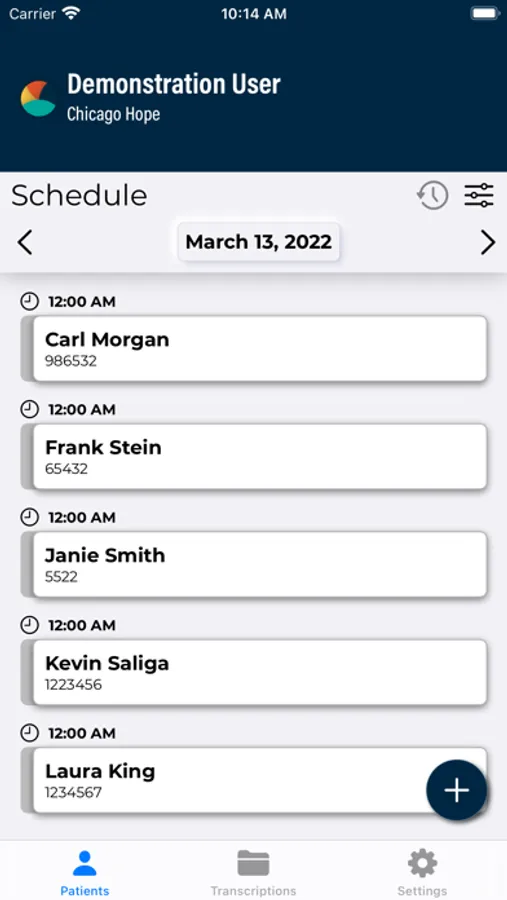
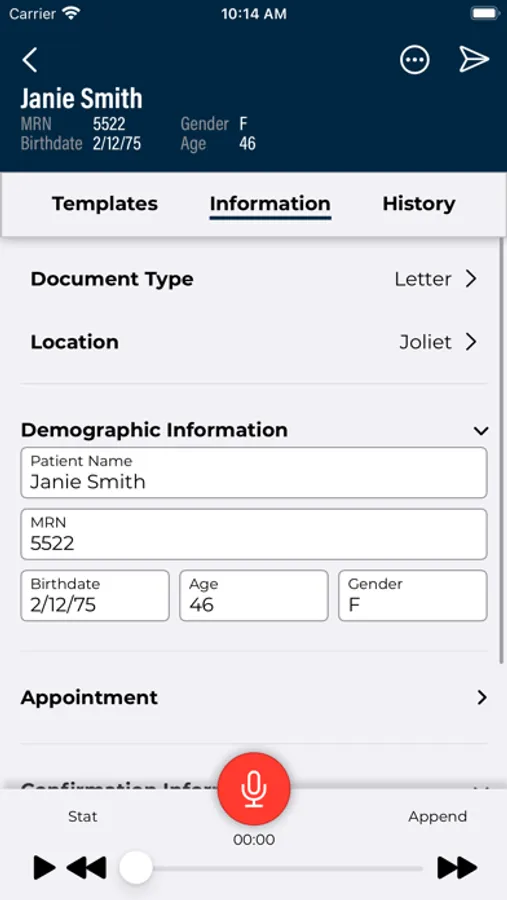
A real-time schedule feed serves as a daily work list while access to patient demographics and history informs dictations. System-generated dictation templates – personalized by each clinician – streamline document creation by requiring only exceptions be dictated. Transcribed content is easily reviewed, edited and signed. Upon completion, uploaded files are automatically integrated into the EMR, faxed, or printed.
REQUIREMENTS:
* Internet access through Wifi or phone service provider is required. WiFi connection is strongly recommended when uploading dictations.
* An account is required to use this application.
FEATURES AND BENEFITS:
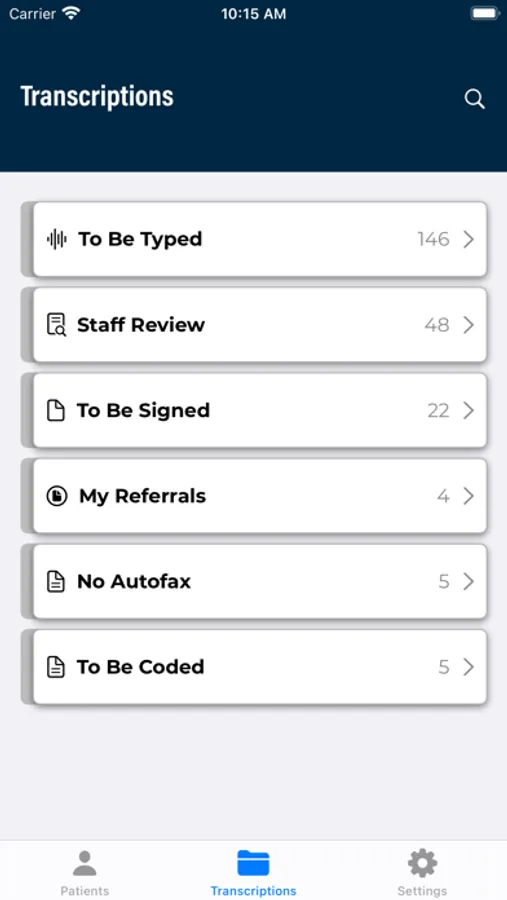
* Manage the documentation task with less time and effort. Clinicians organize documentation tasks across multiple devices by viewing all appointments with dictation status or only appointments still requiring dictation. A list of returned transcriptions allows clinicians to advance quickly through the review and authentication process.
* Improve documentation quality. Save time and remove risk when patient data, demographics and appointment location are automatically linked to the voice file and available for easy reference while dictating.
* Customize workflow to meet clinic needs. Flexible application settings easily accommodate the unique, complex workflow requirements of specialty practices.
* Delegate transcription and QA to support staff. Completed dictations upload in the background and are automatically routed to a professional medical transcriptionist to produce a typed report that is automatically returned for review.
* Increase clinician productivity and satisfaction. A library of templates—customizable for each clinician—automatically populates common content as editable text, speeding dictation.
* Speed documentation turnaround. Real-time file upload, download and routing ensures prompt dictation, transcription, editing, authentication and accessibility in the EMR.
* Populate the EMR automatically. Sophisticated integration generates structured data automatically placed in the EMR, improving EMR usability and boosting adoption and ROI.
* Enhance the patient experience By completing documentation on mobile devices, providers are free to engage with patients rather than computer screens during exams.
* Control documentation costs All-inclusive solution components require no server hardware or infrastructure, eliminating all upfront fees. Unlimited client support, updates and maintenance included at no additional cost.
WHAT CLIENTS ARE SAYING:
“When we introduced our physicians to Emdat Mobile, all of them were amazed by how easy it made their dictation and improved their workflow; and they wanted it right away.”
— William Whelehan, Purchasing Director, Illinois Bone & Joint Institute
A real-time schedule feed serves as a daily work list while access to patient demographics and history informs dictations. System-generated dictation templates – personalized by each clinician – streamline document creation by requiring only exceptions be dictated. Transcribed content is easily reviewed, edited and signed. Upon completion, uploaded files are automatically integrated into the EMR, faxed, or printed.
REQUIREMENTS:
* Internet access through Wifi or phone service provider is required. WiFi connection is strongly recommended when uploading dictations.
* An account is required to use this application.
FEATURES AND BENEFITS:
* Manage the documentation task with less time and effort. Clinicians organize documentation tasks across multiple devices by viewing all appointments with dictation status or only appointments still requiring dictation. A list of returned transcriptions allows clinicians to advance quickly through the review and authentication process.
* Improve documentation quality. Save time and remove risk when patient data, demographics and appointment location are automatically linked to the voice file and available for easy reference while dictating.
* Customize workflow to meet clinic needs. Flexible application settings easily accommodate the unique, complex workflow requirements of specialty practices.
* Delegate transcription and QA to support staff. Completed dictations upload in the background and are automatically routed to a professional medical transcriptionist to produce a typed report that is automatically returned for review.
* Increase clinician productivity and satisfaction. A library of templates—customizable for each clinician—automatically populates common content as editable text, speeding dictation.
* Speed documentation turnaround. Real-time file upload, download and routing ensures prompt dictation, transcription, editing, authentication and accessibility in the EMR.
* Populate the EMR automatically. Sophisticated integration generates structured data automatically placed in the EMR, improving EMR usability and boosting adoption and ROI.
* Enhance the patient experience By completing documentation on mobile devices, providers are free to engage with patients rather than computer screens during exams.
* Control documentation costs All-inclusive solution components require no server hardware or infrastructure, eliminating all upfront fees. Unlimited client support, updates and maintenance included at no additional cost.
WHAT CLIENTS ARE SAYING:
“When we introduced our physicians to Emdat Mobile, all of them were amazed by how easy it made their dictation and improved their workflow; and they wanted it right away.”
— William Whelehan, Purchasing Director, Illinois Bone & Joint Institute