With this health benefits app, you can view claims, manage provider information, and access your virtual ID card. Includes benefits data, pharmacy locations, and customer support contact options.
AppRecs review analysis
AppRecs rating 2.1. Trustworthiness 74 out of 100. Review manipulation risk 22 out of 100. Based on a review sample analyzed.
★★☆☆☆
2.1
AppRecs Rating
Ratings breakdown
5 star
21%
4 star
5%
3 star
3%
2 star
10%
1 star
61%
What to know
✓
Low review manipulation risk
22% review manipulation risk
⚠
Mixed user feedback
Average 2.1★ rating suggests room for improvement
⚠
High negative review ratio
71% of sampled ratings are 1–2 stars
About myBlue
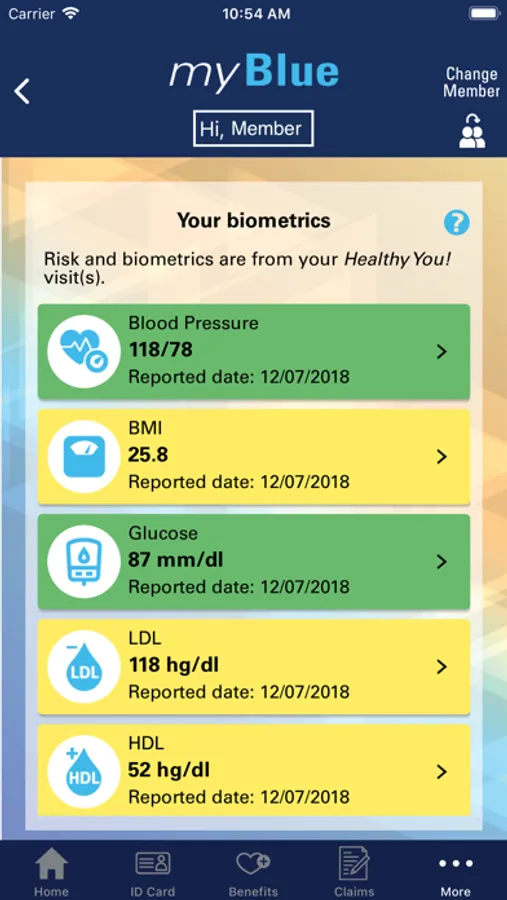
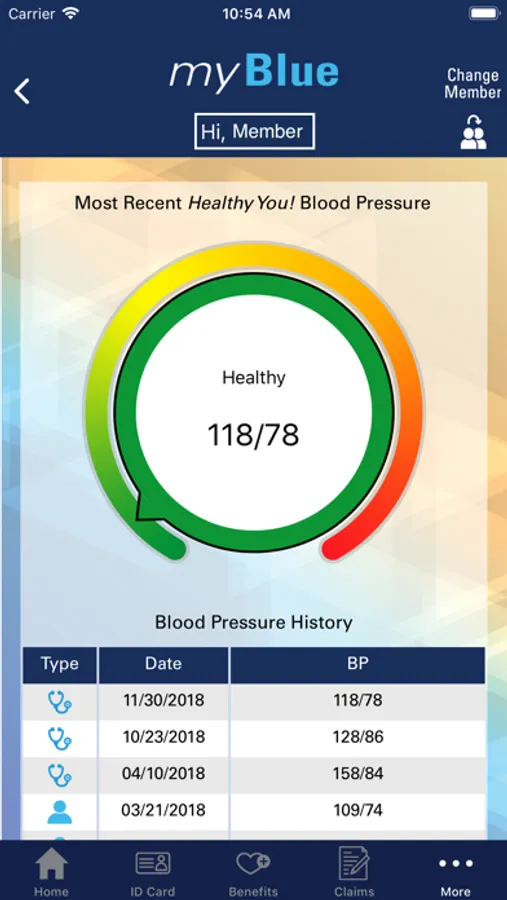
Blue Cross & Blue Shield of Mississippi’s myBlue app gives health and wellness benefit plan members convenient, on-the-go access to their personalized benefit information.
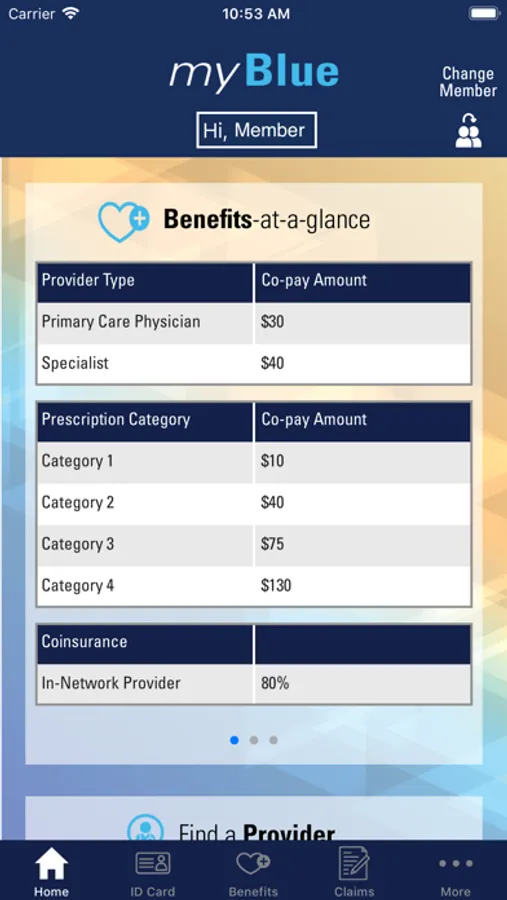
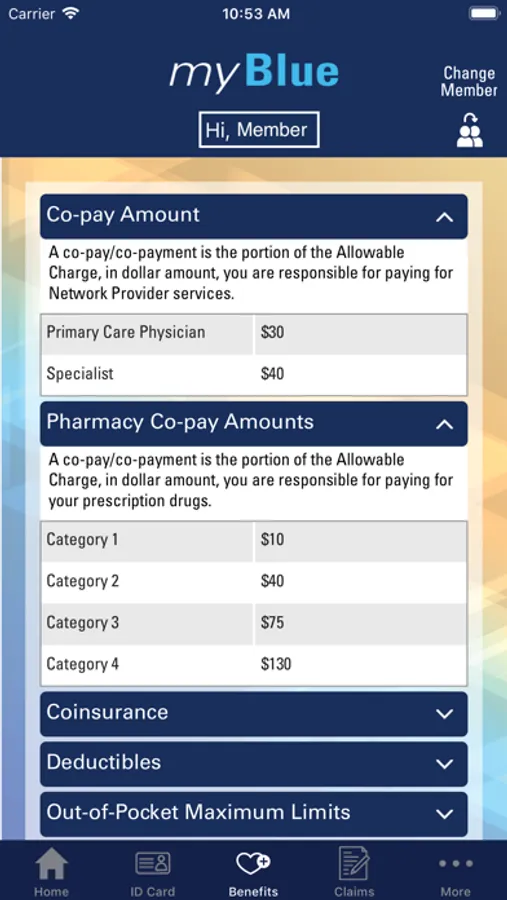
•View benefits “at a glance” including provider and prescription drug co-pays, deductibles and coinsurance.
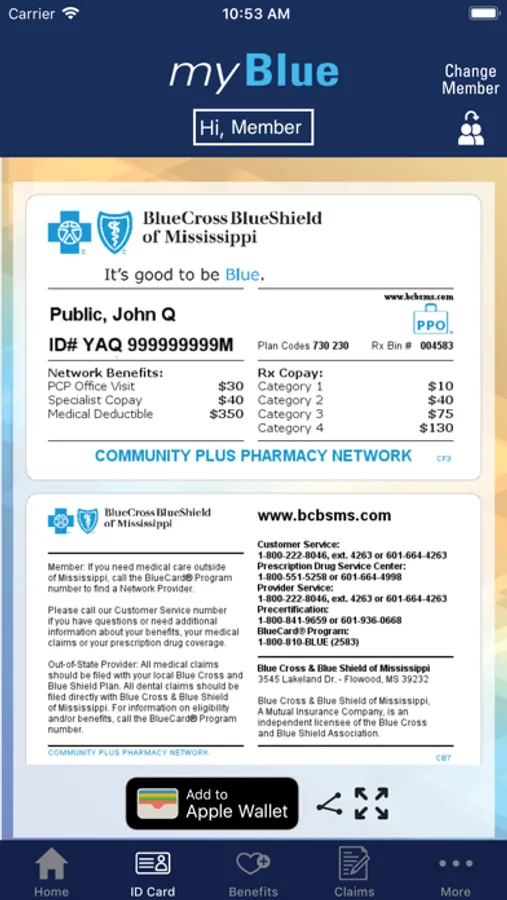
•Never worry about leaving your ID card at home with the virtual ID Card.
•View 15 months of claims history as soon as they are paid.
•Find prescription drug information, including claims, co-pays and lower cost alternatives.
•Review biometric numbers and related health risk levels.
•Check wellness and health management benefits.
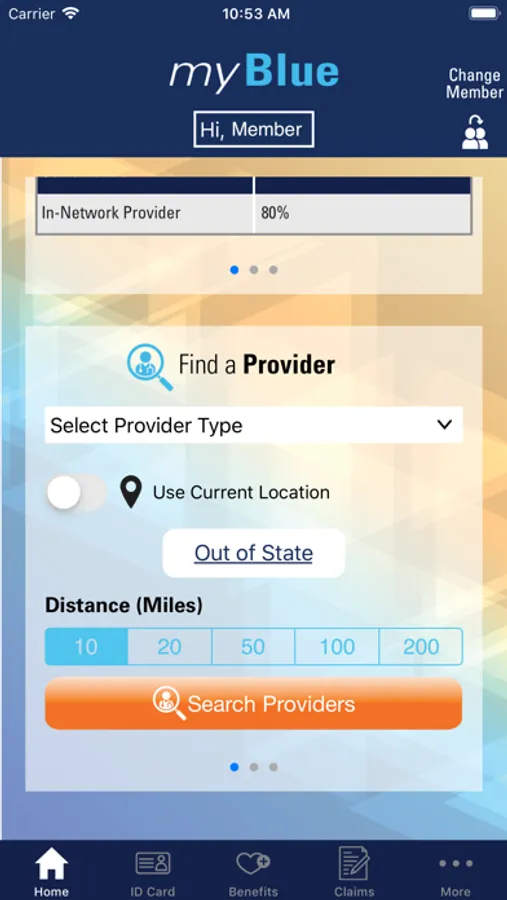
•Search for a Network Provider, map their location and call their office with one touch.
•Update personal contact information.
•Locate a Community PLUS Network Pharmacy, including those open 24 hours.
Members can also quickly and easily connect to a member of our Customer Support Team.
The myBlue app is one more reason why now, more than ever, it’s good to be Blue!
Contact us at 601-664-4590 or 800-942-0278, Monday through Friday, 8:00 a.m. to 4:30 p.m. Central time or visit bcbsms.com for more information.
*Available only for Blue Cross & Blue Shield of Mississippi members
•View benefits “at a glance” including provider and prescription drug co-pays, deductibles and coinsurance.
•Never worry about leaving your ID card at home with the virtual ID Card.
•View 15 months of claims history as soon as they are paid.
•Find prescription drug information, including claims, co-pays and lower cost alternatives.
•Review biometric numbers and related health risk levels.
•Check wellness and health management benefits.
•Search for a Network Provider, map their location and call their office with one touch.
•Update personal contact information.
•Locate a Community PLUS Network Pharmacy, including those open 24 hours.
Members can also quickly and easily connect to a member of our Customer Support Team.
The myBlue app is one more reason why now, more than ever, it’s good to be Blue!
Contact us at 601-664-4590 or 800-942-0278, Monday through Friday, 8:00 a.m. to 4:30 p.m. Central time or visit bcbsms.com for more information.
*Available only for Blue Cross & Blue Shield of Mississippi members